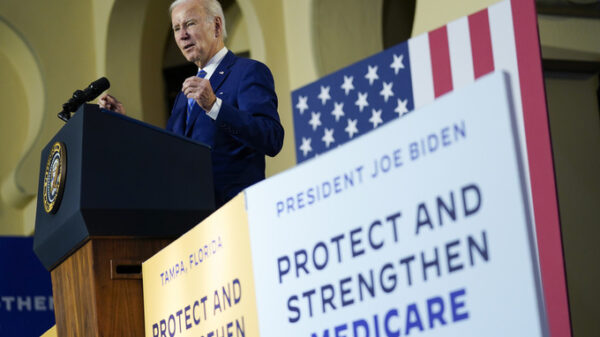
Mobile Emergency Care Service (SAMU) bring Binta Ba, who is eight months pregnant and has COVID-19, to the hospital in Dakar, Senegal, Friday, Aug. 6, 2021. Ambulance services in the West African nation of Senegal say about 90% of their calls right now are responding to COVID-19 patients with trouble breathing. The avalanche of cases comes as Senegal confronts a devastating third wave with the arrival of the delta variant. (AP Photo/Leo Correa)
DAKAR, Senegal (AP) — The paramedics get the urgent call at 10:30 p.m.: A 25-year-old woman, eight months pregnant and likely suffering from COVID-19, is now having serious trouble breathing.
Yahya Niane grabs two small oxygen cylinders and heads to the ambulance with his team. Upon arrival, they find the young woman’s worried father waving an envelope in front of her mouth, a desperate effort to send more air her way.
Her situation is dire: Niane says Binta Ba needs to undergo a cesarean section right away if they are to save her and the baby. But first they must find a hospital that can take her.
“All the hospitals in Dakar are full so to find a place for someone who is having trouble breathing is very difficult,” he says.
It’s a scenario that has become all too common as Senegal confronts a rapid increase in confirmed coronavirus cases. Instead of motorcycle accidents and heart attacks, the vast majority of ambulance calls in the country’s capital are now COVID-19 cases.
“We have had an influx of calls for respiratory distress,” said Dr. Abdallah Wade, head of the regulation department at SAMU, Senegal’s emergency medical service. “We had a few in the first wave, a few in the second wave, but since the beginning of the third wave, 90% of the calls are for respiratory distress.”
During the first year of the pandemic, Senegal was frequently cited as a success story in Africa: After quickly closing the country’s airport and land borders, President Macky Sall mandated mask-wearing and temporarily halted interregional travel.
The delta variant, though, has changed all that. While the country of 16 million people received more 500,000 AstraZeneca vaccines through the U.N.-backed COVAX initiative, the demand has now outstripped the supply leaving many still waiting for their second doses.
Hospital beds, too, are in short supply, leaving COVID-19 patients to languish at home while they wait for a spot or until their condition further deteriorates.
“Now there is an overflow of calls and an overflow of patients and very few places available,” said Dr. Mouhamed Lamine Dieng, who works at the emergency services control center trying to triage and place patients.
“The main challenge for the team is to find a place at the right time to save a person before they die,” he said.
Binta Ba, the young expectant mother, ultimately got a spot since her oxygen levels had dropped sharply. Doctors estimated that 50% of her lungs had been affected by the virus by the time she made it there.
Doctors delivered her baby girl by cesarean in time. Four days later though, the mother remains on oxygen support in the intensive care unit while hospital workers tend to the newborn.
“There are people who thought that COVID did not exist,” said Djiba Ba, the baby’s grandfather.
“This is because some people denied its existence on social media networks and TV channels,” he said. “I swear to you that COVID is real and that people who refuse to be vaccinated should be punished.”
Copyright 2020 Associated Press. All rights reserved.